|
Antiretroviral Clinical Trials – Breaking News
Immunologic Biomarkers, Morbidity, and Mortality in Treated HIV Infection
Hunt P et al.
J Infect Dis. 2016 Oct 1;214 Suppl 2:S44-50
14th December 2016, by Dr Anton Pozniak
Despite marked improvements in the modern treatment era, HIV–infected individuals, particularly those who initiated ART at advanced disease stages, continue to have increased age-related morbidity and mortality, compared with the general population. Immune activation and inflammation persist despite suppressive ART and predict many of these morbidities. This review examines the evidence suggesting a link between the persistent inflammatory state and morbidity and mortality in this setting, describes the impact of early ART initiation on these factors, and highlights important unanswered questions for the field. We also advance a hypothesis to explain why some morbidities, and their root inflammatory drivers, may be prevented more than others by early ART initiation.
Inflammation is likely to be a more important contributor to morbidity and mortality in the context of HIV infection than it is in the general population.
Recent observational studies demonstrated a strong link between lower nadir CD4+
T-cell count and cardiovascular disease risk in HIV-infected individuals and other studies suggested that the relative risk of cardiovascular disease (CVD) among HIV-infected individual as compared to the general population has been declining as the median CD4+ T-cell count at ART initiation has been rising.
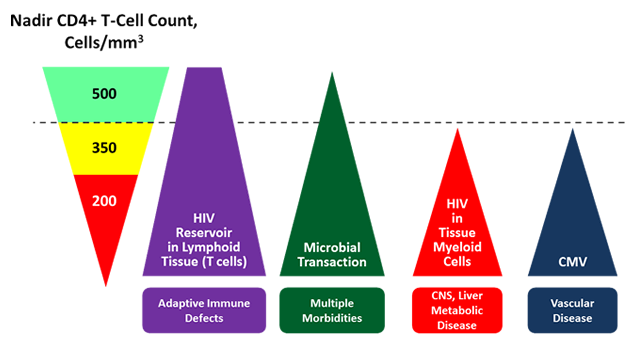
FIGURE: hypothesis related to the distinct putative drivers of immune activation during ART-mediated viral suppression, their relationship to the degree of pre-ART immunodeficiency (ie, nadir CD4+ T-cell count), and their anatomic localization
- viral reservoirs in central memory T-cell compartments, which are most abundant in inductive lymphoid tissues, are established within the first several days of systemic HIV infection, with an exponential increase in the first few weeks of infection followed by slower increases over the next few years. Once ART-mediated viral suppression is established, this primarily T-cell reservoir of HIV persists in lymphoid tissues and likely contributes to ongoing inflammation and lymphoid fibrosis, which may plausibly contribute to adaptive immune defects since these responses normally develop in the same anatomic compartment. Since immediate ART fails to eliminate T-cell reservoirs of HIV in lymphoid tissues, may explain the persistently high incidence of infectious and neoplastic complications receiving immediate ART.
- markers of microbial translocation are evident in plasma within the first few weeks of HIV infection, the degree to which these defects become irreversible after ART-mediated viral suppression is greater with more-advanced disease. While translocated microbial products are concentrated in the liver and mesenteric lymphoid tissues, they are distributed widely throughout the circulation, so this driver of the systemic inflammatory state may plausibly contribute to several end-organ diseases, including CV complications, particularly in individuals with lower nadir CD4+ T-cell counts.
- Other potential drivers of the inflammatory state may require significant pre-ART immunodeficiency to be established and have distinct anatomic localization. For example, myeloid reservoirs of HIV in tissues (eg, brain microglia, adipose tissue, and liver), if they do persist during suppressive ART, might not be established to a clinically meaningful extent until later stages of untreated HIV infection because it appears to take some degree of CD4+ T-cell depletion for the virus to evolve the capacity to efficiently
infect myeloid cells. This might explain why irreversible neurocognitive dysfunction, which is thought to be driven in part by direct HIV infection of central nervous system myeloid cells, appears to be much less common in individuals who initiate ART at high nadir CD4+ T-cell counts. Myeloid reservoirs of HIV in fat and liver might also plausibly contribute to metabolic disease and liver fibrosis in individuals with low nadir CD4+ T-cell counts .
- Asymptomatic CMV replication, which has been proposed to be a mediator of CV disease in HIV-infected individuals, particularly since it replicates in the vascular endothelium, may require a certain degree of immunodeficiency to establish sufficient CMV reservoirs in myeloid precursors or CMV-specific adaptive immune defects to drive CVD.
Consequently, both the root drivers of inflammation reflected by systemic biomarker measurements and the disease manifestations induced by inflammation are likely to vary on the basis of nadir CD4+ T-cell count. This model might explain why individuals initiating ART during early disease stages may prevent the establishment of certain (eg, CV, neurocognitive, and pulmonary) morbidities but still have a measurably increased risk of infectious and neoplastic morbidities as compared to the general population.
Conclusion:
While the life expectancy of HIV-infected individuals has extended dramatically in the modern treatment era, non–AIDS-defining morbidity and mortality remains higher than in the general population, particularly among individuals who initiate ART at low nadir CD4+ T-cell counts. Abnormal immune activation and inflammation persist despite ART-mediated viral suppression and are associated with several non–AIDS-defining morbidities, but most of these data linking inflammatory biomarkers to morbidity have been generated in cohorts of HIV-infected individuals with relatively low nadir CD4+ T-cell counts. It remains to be seen whether the inflammatory state, which persists even among those who initiate ART in the first few weeks of HIV infection, will continue to predict all morbidities or a more narrow spectrum of infectious and neoplastic conditions in HIV-infected individuals who initiate ART early in the disease course. If this were the case, it would have important implications for the target populations (and end-organ diseases of interest) in need of immune-based interventions, as well as the specific root drivers of the inflammatory state to be targeted. Nevertheless, despite changing international guidelines supporting ART initiation at any CD4+ T-cell count, the majority of HIV-infected individuals around the world will have (now and in the foreseeable future) initiated ART at low CD4+ T-cell counts and remain at risk for multiple end-organ diseases as a consequence of the systemic inflammatory state. In addition, given the continued marked infectious morbidity among HIV-infected individuals initiating ART at high CD4+ T-cell counts in these resource-limited settings, immune-based interventions to reverse adaptive immune defects will play an important role in this population, as well.
|



