Switch studies in virologically suppressed patients
Switch to LPV/r monotherapy
OK04 Study: Switch LPV/r + 2NRTIs to LPV/r monotherapy
Original article : AIDS. 2008 Jan 11;22(2):F1-9 – F Pulido ; J Acquir Immune Defic Syndr. 2009 Jun 1;51(2):147-52 – JR Arribas
Last update :
28/03/2014
Dr Anton Pozniak
Chelsea and Westminster Hospital
London, UK

- From W48 data
- In patients with virologic suppression for more than 6 months on LPV/r + 2 NRTIs, LPV/r monotherapy followed by re-introduction of the NRTIs as required is a therapeutic strategy as effective as continuing triple therapy: non inferiority of monotherapy was demonstrated
- The vast majority of patients with loss of virologic suppression�on LPV/r monotherapy had no evidence of resistance mutations in the protease gene and were able to resupress and maintain virologic suppression after resumption of baseline NRTIs
- From W96 data
- The 96 weeks results support the efficacy and safety of the�LPV/r monotherapy strategy
- Although episodes of low-level viremia were more frequent in�the monotherapy group, there was not an increased risk of resistance development and most of these patients could be virologically resupressed with addition of NRTIs
- The toxicity of the LPV/r monotherapy regimen was lower than the toxicity of the triple regimen

Design :
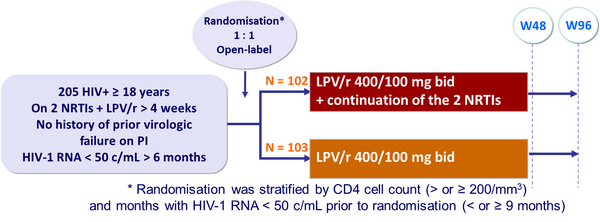
Objective :
- Non inferiority of the monotherapy group in the proportion of patients with therapeutic failure at W48 (per-protocol analysis) ; upper limit of the 95% CI�for the difference = 12%, 80% power
- Therapeutic failure: 2 consecutive HIV-1 RNA > 500 c/mL (if no resistance at failure and successful viral suppression after reintroduction of 2 NRTIs, not considered as failure) ; change of randomised therapy ; treatment discontinuation ; loss to follow-up
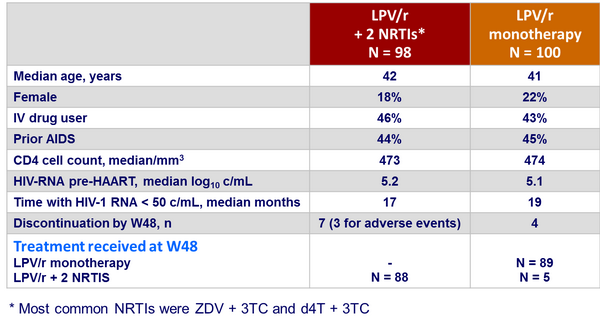
Baseline characteristics and patient disposition :
Outcome at week 48 :
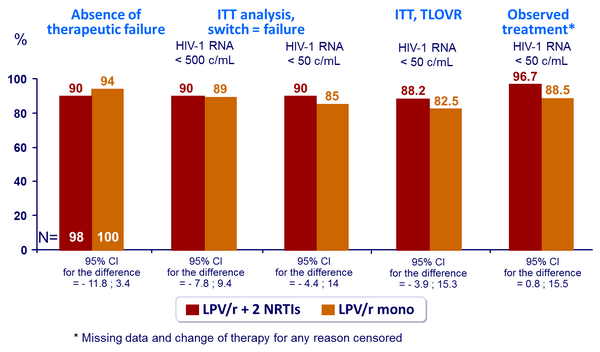
Response to treatment at week 48 :
- Therapeutic failures
- 6 in the monotherapy group
- 3 were lost to follow-up
- 1 changed randomised therapy without loss of virologic suppression
- 1 lost virologic suppression and developed PI resistance
- 1 lost virologic suppression and failed to achieve suppression after reintroduction �of NRTIs
- 10 in the triple therapy arm
- 4 were lost to follow-up
- 3 had confirmed loss of virologic suppression
- 3 discontinued randomised treatment due to adverse events
- Loss of virologic suppression at W48
- 3 in the triple therapy group
- 6 in the monotherapy group: of these 6, 4 resumed baseline NRTIs and regained virologic suppression, 1 had LPV/r resistance, and 1 did not achieve virologic suppression after resuming baseline NRTIs
Safety, Adverse events, Resistance, Adherence (W48) :
- Study drug-related adverse events of at least moderate severity
- 3 in the triple therapy group (diarrhoea, N = 2, insomnia, N = 1), �leading to treatment discontinuation
- None in the monotherapy group (p = 0.08)
- No statistical significant changes from baseline in fasting total cholesterol, HDL cholesterol or triglycerides in both groups
- Genotypic analysis in patients with HIV-1 RNA > 500 c/mL
- 3 in the triple therapy group:
- PI resistance, N = 1 (mutations 54V, 63P, 71V and 82A)
- NRTI resistance, N = 1
- 11 in the monotherapy group:
- PI resistance, N = 2 (mutations 10F and 46I in 1 ; mutations 54V, 77I and 82A in 1)
- NRTI resistance, N = 1
- No difference in adherence between the 2 groups
-
Outcome at week 96 :
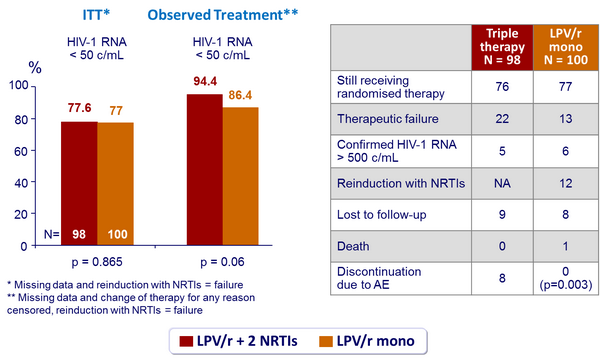
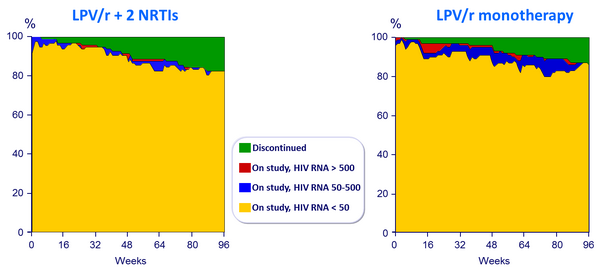
Point prevalence of discontinuations and virologic response through 96 weeks :
- After 2 years of follow-up, proportion of patients rebounding with isolates containing major PI mutations was 2% in each group
 Back to Table of Contents Back to Table of Contents
|



