Switch studies in virologically suppressed patients
Switch to RAL-containing regimen
EASIER Study: Switch ENF to RAL
Original article : Clin Infect Dis. 2009 Oct 15;49(8):1259-67 – N De Castro ; J Antimicrob Chemother. 2011 Sep;66(9):2099-106 – S Gallien ; J Infect Dis. 2013 Sep;208(6):892-7 – EF Silva
Last update :
28/03/2014
Dr Anton Pozniak
Chelsea and Westminster Hospital
London, UK

- From W24 data
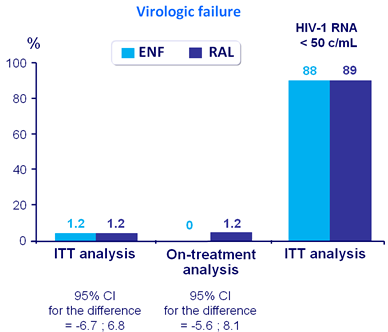
- In patients infected with multidrug-resistant HIV-1 receiving suppressive enfuvirtide-containing antiretroviral therapy, a�switch from enfuvirtide to RAL is:
- Safe
- Well-tolerated
- And virologically non-inferior to the maintenance of ENF

Design :
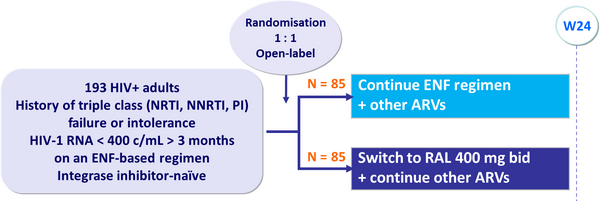
Objective :
- Non inferiority in the proportion of patients with virologic failure at W24�(Intent-to-treat analysis) ; upper limit of the 95% CI for the difference =�10%, 80% power
- Virologic failure : confirmed HIV-1 RNA ≥ 400 c/mL, or a single�HIV-1 RNA ≥ 400 c/mL followed by treatment modification or last �HIV-1 RNA ≥ 400 c/mL without confirmation
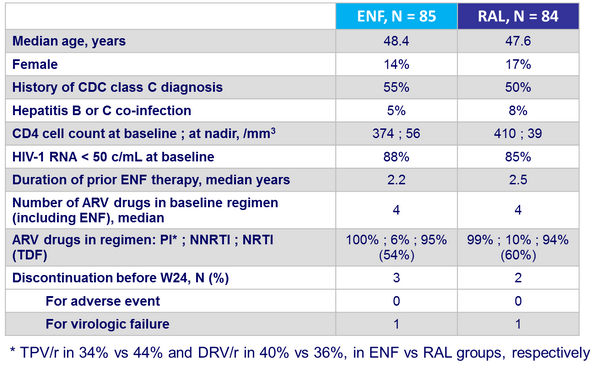
Baseline characteristics and patient disposition :
Outcome at week 24 :
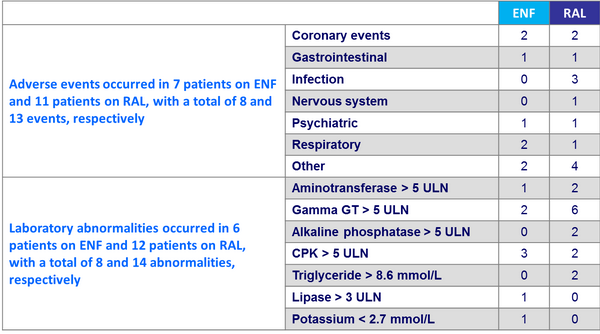
Other endpoints
- Median CD4 increase
- ENF: +15/mm3
- RAL: +11/mm3
- No AIDS events
- No difference in the overall incidence of adverse reactions between both groups
- Higher incidence of grade 1 to 4 laboratory abnormalities in the RAL arm (p = 0.001)
- Median increases in triglycerides and total cholesterol were significantly higher in the RAL group
Grade 3 or 4 emerging adverse events or laboratory abnormalities :
At week 24
- ENF arm switched to RAL (deferred RAL), n = 84
- RAL arm continued on RAL (immediate RAL), n = 84�
Week 48 analyses
- Primary : cumulative proportion of patients with confirmed �HIV RNA ≥ 400 c/mL, or last HIV RNA ≥ 400 c/mL or treatment change after a single HIV RNA ≥ 400 c/mL (on-treatment and intent-to-treat analyses)
- Secondary
- Proportion of patients with HIV RNA < 50 c/mL
- Emergence of resistance in patients with virologic failure
- Changes from baseline in CD4 cell counts
- Proportion of patients with permanent discontinuation of RAL
- Safety
Baseline GSS assessed on cumulative historical genotypes
- GSS ≥ 1 : 86% ; 0.5 : 11% ; 0 : 3% (n = 5)
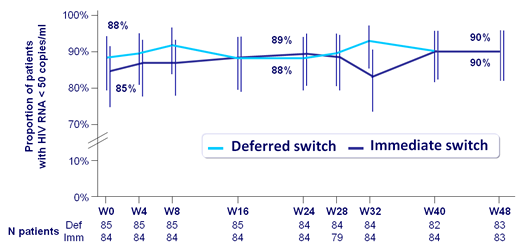
- On-treatment analysis : 1 virologic failure (W8) in immediate arm ; baseline GSS = 0,�no emergence of RAL-associated resistance mutations
- No significant changes in the median CD4 cell counts following RAL switch in either arm
- No significant changes between baseline and W48 in glucose levels or fasting lipids�in either arm
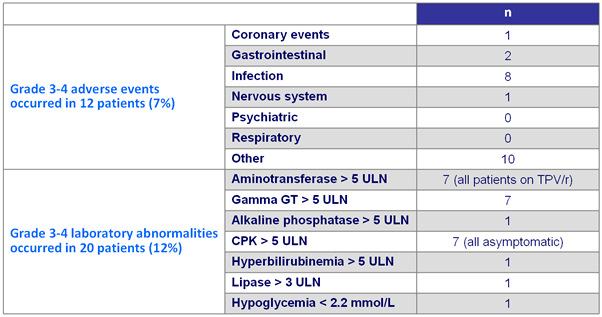
Grade 3 or 4 emerging adverse events or laboratory abnormalities In both arms between weeks 24 and 48 (N = 168) :
EASIER substudy: Inflammatory and coagulation biomarkers
- 164 patients, Immediate switch (n = 83) ; deferred switch (n = 81)
- Biomarkers
- Primary objective : changes in IL-6, hsCRP and D-dimer plasma levels from baseline to W24 between the immediate and deferred arms
- Log10 transformation of levels
- Median changes from baseline assessed by 1-sample t tests
- Comparison between arms used 2-sample t tests with no adjustment for baseline factors
- Similar analyses to compare changes from baseline to W48
 Back to Table of Contents Back to Table of Contents
|



